Contents
- 1 A Proposition of Innovative Curricula for Traditional and Accelerated Medical Schools
- 2 Prof. Aécio D’Silva, Ph.D AquaUniversity
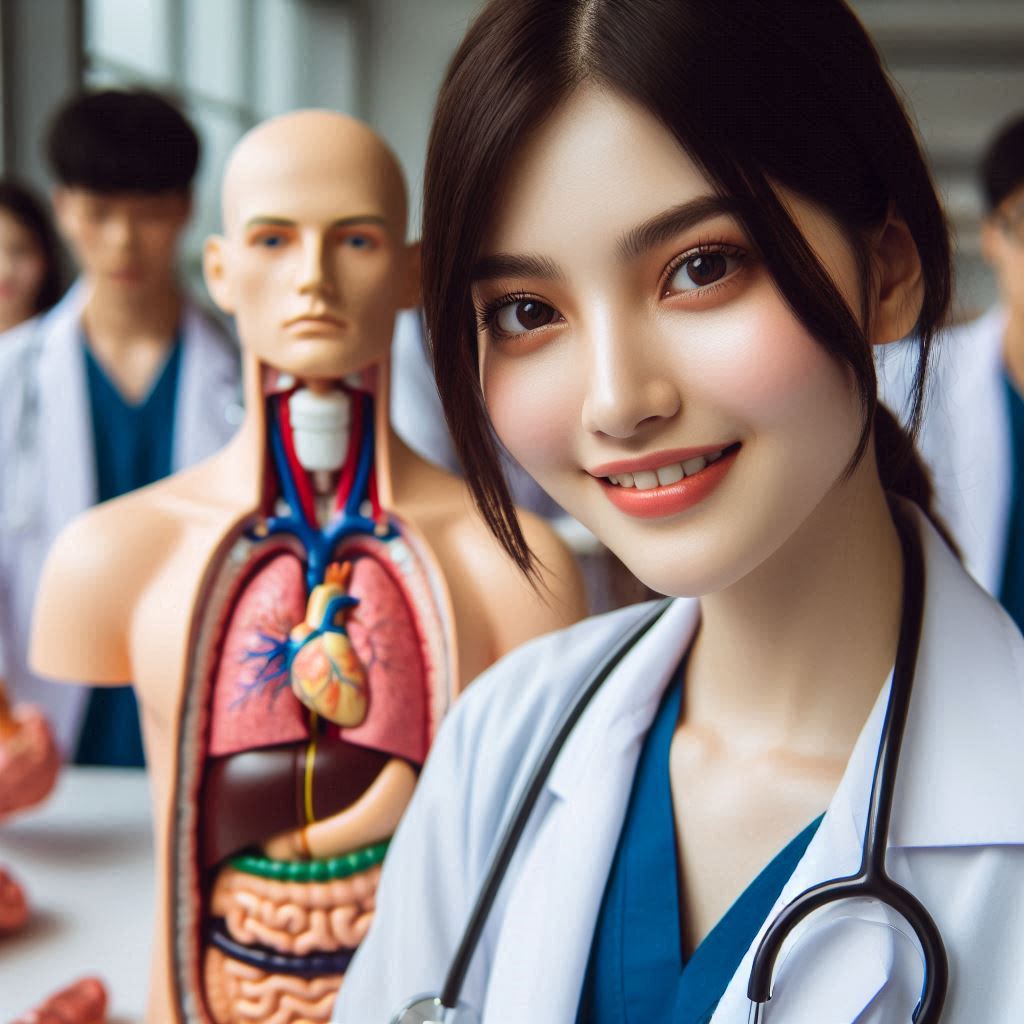
- 3 State-of-the-art digital e-learning platforms and simulation labs maximize the training of medical students, symbolizing a rich educational experience in innovative medical schools
- 4 Medical education – E-learning Platforms and Simulation Labs will revolutionize medical education
- 5
- 6 Medical education – What specific skills can medical students develop through simulation labs?
- 7
- 8 Medical education – How simulation labs exponentiate learning outcomes:
- 9 Medical education – How do simulation labs adapt to new medical procedures and technologies:
- 10 Medical Education – Considerations for Building a Simulation Lab in Medical Education
- 11 Medical education – Robotic Surgery: What It Is, Examples, Benefits & Risks
- 12
- 13 Medical education – Outline of Normal Medical Education Program (6-7 Years)
- 14 Medical education – Outline of Accelerated Medical Education Program (3-4 Years)
A Proposition of Innovative Curricula for Traditional and Accelerated Medical Schools
Prof. Aécio D’Silva, Ph.D
AquaUniversity
State-of-the-art digital e-learning platforms and simulation labs maximize the training of medical students, symbolizing a rich educational experience in innovative medical schools
Medical education must be based on an innovative curriculum and modern teaching systems such as digital platforms, simulation laboratories, and medical robots. This intelligent combination offers an exceptional methodology of rigorous academic training and practical clinical experience. In this article, we propose the implementation of a curriculum designed to produce competent, innovative, and compassionate doctors. With these guidelines, these medical schools will gain recognition from the community for their creative approach to medical training. This intelligent collaborative post lays out the foundation for creating typical components, subjects, course lengths, and specialization options for a 21st-century medical school curriculum.
Medical education – E-learning Platforms and Simulation Labs will revolutionize medical education
Let’s begin by highlighting a crucial aspect to be integrated into current medical teaching practices. Both newly established and existing schools must prioritize the use of e-learning platforms and simulation laboratories, as these techniques are radically transforming medical education in the current and the near future. This revolution is due to their accessibility and lower cost of investments and implementation.
Here are some key points and the immense benefits of utilizing e-learning platforms and simulation labs to increase learning efficiency and enhance the practical skills of medical students in medical education:
e-Learning Platforms:
Accessibility: E-learning platforms can provide high-quality medical education to a broader audience, regardless of geographical location. This is especially advantageous for students in remote or underserved areas who may lack access to traditional medical schools.
Flexibility: E-learning allows students to access educational materials at their own pace and convenience. This flexibility accommodates different learning styles and enables students to balance their studies with other commitments such as work or family obligations.
Interactive Learning: E-learning platforms can incorporate interactive multimedia elements such as videos, animations, simulations, and quizzes, making the learning process more engaging and effective. These interactive tools help students better understand complex medical concepts and procedures.
Self-assessment: E-learning platforms often include self-assessment tools such as quizzes and practice exams, allowing students to gauge their understanding and identify areas needing further study. This promotes active learning and helps students take ownership of their education.
Remote Collaboration: E-learning facilitates collaboration among students and educators, enabling communication and teamwork through discussion forums, online chat, video conferencing, and other digital tools. This fosters a sense of community and allows for peer-to-peer learning and collaboration on group projects.
Access to Resources: E-learning provides students with a wide range of educational resources, including digital textbooks, journal articles, case studies, and online databases. This ensures students stay up-to-date with the latest advancements in medical research and practice.
Continuing Medical Education (CME): E-learning platforms are valuable for continuing medical education, allowing practicing physicians to stay current with advances in their field, fulfill continuing education requirements, and maintain their professional competence throughout their careers.
Cost-Effectiveness: E-learning can be more cost-effective than traditional classroom-based education, eliminating the need for physical infrastructure and reducing expenses related to travel and accommodation. This makes medical education more accessible and affordable for students.
Simulation labs:
- Realistic scenarios: Simulation labs provide realistic patient scenarios that closely resemble actual clinical encounters. Students can practice assessing patients, making clinical judgments, prioritizing care, and performing interventions in a controlled environment.
- Safe learning environment: Simulation labs offer a risk-free space for students to make mistakes and learn from them without compromising patient safety. This allows students to experiment, take risks, and develop proficiency.
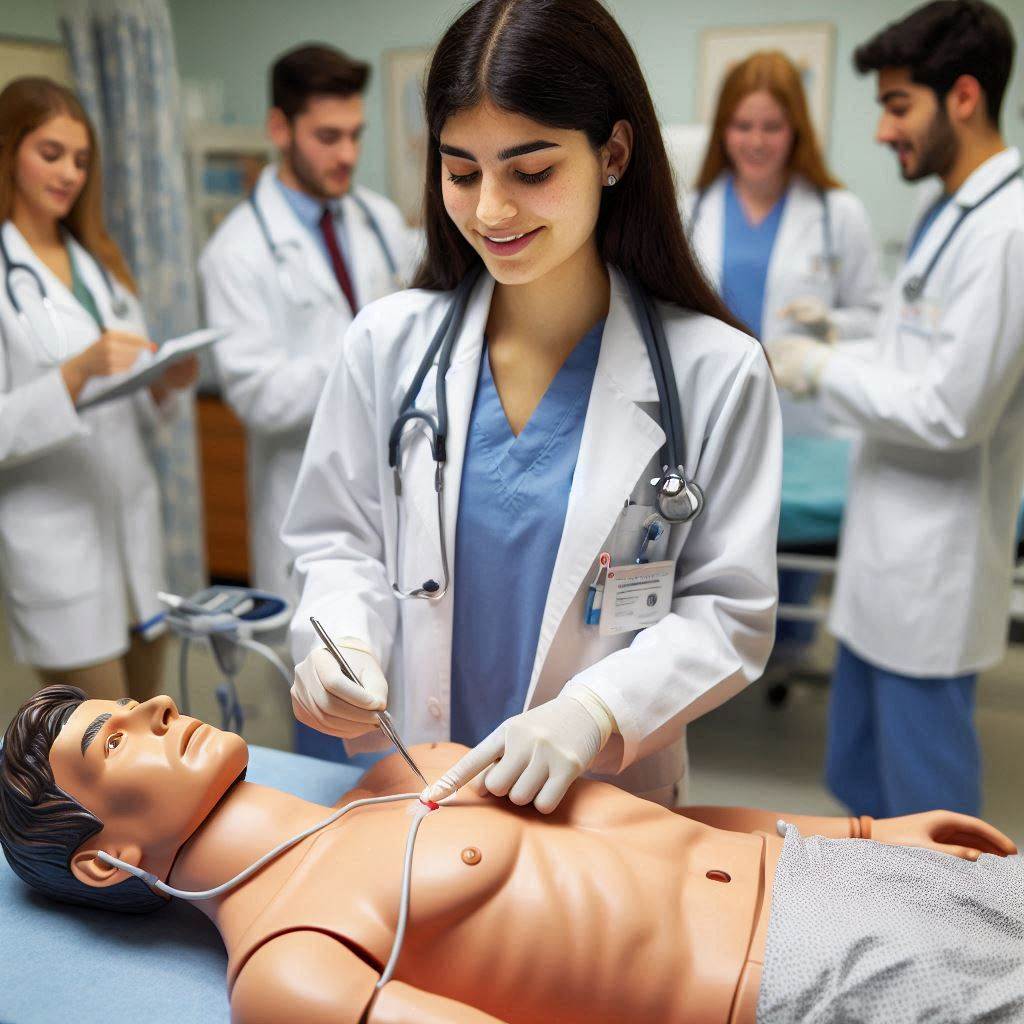
- Hands-on practice: Students can practice clinical skills like administering medications, performing procedures, and communicating with patients using high-fidelity mannequins and medical equipment.
- Immediate feedback: Instructors can provide personalized, real-time feedback on students’ performance. This allows for deliberate practice and improvement of specific skills.
- Exposure to rare cases: Simulation labs can recreate rare or critical scenarios that students may not encounter frequently in clinical rotations.
- Teamwork and communication: Interprofessional scenarios allow students to practice collaborating with other healthcare professionals, improving teamwork and communication skills.
- Building confidence: Repeated practice in realistic settings helps students build confidence in their abilities before working with real patients.
- Standardized assessment: Simulation labs provide a standardized way to assess students’ clinical competencies using objective measures.
- Bridging theory and practice: Labs help students apply theoretical knowledge to practical clinical situations.
- Patient safety focus: Students learn to prioritize patient safety and practice error prevention in a controlled setting.
- Technology familiarity: Students gain experience with medical equipment and technology they’ll use in real clinical environments.
Medical education – What specific skills can medical students develop through simulation labs?
Technical clinical skills: Students can practice hands-on skills like phlebotomy (take blood from a vein), IV placement, physical examinations, and other procedures in a safe environment.
- Communication skills: Simulation scenarios allow students to practice communicating with “patients” (mannequins or actors) and other healthcare team members.
- Critical thinking and clinical reasoning: Students must assess situations, make diagnoses, and determine appropriate treatments in simulated scenarios.
- Decision-making skills: Simulations require students to make quick decisions under pressure, similar to real clinical environments.
- Teamwork and collaboration: Many scenarios involve working in teams, helping students learn to coordinate care with others.
- Leadership skills: Students may take on distinct roles in scenarios, including leadership positions.
- Situational awareness: Simulations help students learn to monitor and understand everything happening in a clinical environment.
- Error prevention and patient safety practices: Students can make mistakes and learn from them without risking real patient harm.
- Time management and prioritization: Scenarios often involve multiple tasks that must be prioritized and managed efficiently.
- Professionalism and ethical decision-making: Students can practice navigating challenging ethical situations in a controlled setting.
- Confidence building: Repeated practice in realistic scenarios helps build students’ confidence in their abilities.
- Stress management: Simulations help students learn to perform under pressure and in high-stress situations.
- Use of medical equipment: Students gain familiarity with various medical devices and technologies used in clinical settings.
- Documentation skills: Many simulation labs incorporate practice with electronic health records and other documentation systems.
- Debriefing and self-reflection: Post-simulation discussions help students develop skills in analyzing their own performance and learning from experiences.
These skills are developed through deliberate practice, immediate feedback, and the opportunity to gain experience from mistakes in a safe, controlled environment. Simulation labs bridge the gap between classroom learning and real clinical practice, helping prepare students more effectively for their future roles as healthcare providers.
By providing these enhanced learning experiences, simulation labs help prepare medical students to deliver high-quality, safe patient care when they enter really clinical practice.
Medical education – How simulation labs exponentiate learning outcomes:
Here’s an exhibit on how simulation labs exponentiate learning outcomes:
- Safe learning environment: Students can practice skills and make mistakes without risking patient safety.
- Controlled scenarios: Instructors can create specific situations to target particular learning objectives.
- Repeated practice: Students can practice procedures multiple times to gain proficiency.
- Immediate feedback: Instructors can provide real-time feedback and guidance.
- Exposure to rare cases: Simulation labs can recreate rare or critical scenarios that students may not encounter frequently in clinical rotations.
- Standardized experiences: All students can be exposed to the same scenarios, ensuring consistent learning opportunities.
- Technology integration: Students can gain familiarity with medical equipment and technology in a low-pressure environment.
- Interprofessional training: Simulation labs allow for team-based scenarios involving multiple healthcare disciplines.
Medical education – How do simulation labs adapt to new medical procedures and technologies:
Here are some key ways that simulation labs adapt to new medical procedures and technologies:
- Regular updates to equipment and technology: Simulation labs strive to keep their equipment and technology up-to-date to reflect what students will encounter in real clinical settings. This includes acquiring new medical devices, updating software, and incorporating emerging technologies like virtual reality and augmented reality.
- Modular and flexible design: Many simulation labs are designed with flexibility in mind, allowing for easy reconfiguration of spaces to accommodate new procedures or equipment. This modular approach enables labs to adapt quickly to changing needs.
- Collaboration with medical device companies: Simulation labs often partner with medical device manufacturers to incorporate the latest equipment and technologies into their training programs. This ensures students are familiar with cutting-edge tools and procedures.
- Continuous curriculum development: Simulation lab staff and educators regularly review and update their training scenarios and curricula to include new procedures, best practices, and emerging medical knowledge.
- Integration of advanced technologies: Labs are increasingly incorporating technologies like 3D printing, artificial intelligence, and robotics to simulate complex procedures and enhance learning experiences.
- Multidisciplinary approach: Simulation labs often involve experts from various medical specialties to ensure that new procedures and technologies are accurately represented across different areas of healthcare.
- Feedback and iterative improvement: Many labs use feedback from students, instructors, and healthcare professionals to continuously improve and adapt their simulation experiences.
- Investment in faculty development: Simulation labs invest in training their staff and faculty to stay current with new medical procedures and technologies, ensuring they can effectively teach and assess students using the latest methods.
- Partnerships with healthcare institutions: Collaboration with hospitals and clinics helps simulation labs stay informed about the latest practices and technologies used in real-world settings.
- Adaptable software systems: Many modern simulation labs use software platforms that can be easily updated to incorporate new scenarios, procedures, and technologies without requiring a complete overhaul of the system.
By employing these strategies, simulation labs can remain agile and responsive to the rapidly evolving landscape of medical procedures and technologies, ensuring that students receive the most up-to-date and relevant training possible.
Medical Education – Considerations for Building a Simulation Lab in Medical Education
Designing and constructing a simulation lab for medical education is a complex process that requires careful planning and collaboration. Here’s a comprehensive guide to the key considerations:
- Stakeholder Involvement
-
- Engage all relevant departments early in the planning process, including:
-
-
- Facilities management
- Information Technology (IT)
- Pharmacy
- Clinical departments
-
-
- This collaborative approach ensures that all perspectives are considered and potential issues are addressed proactively.
- Learning Objectives and Target Audience
-
- Clearly define the intended learning outcomes
- Identify the level of learners (e.g., medical students, residents, practicing physicians)
- Align the lab design with curriculum needs and accreditation requirements
- Budget and Space Allocation
-
- Determine the available budget for initial setup and ongoing operations
- Assess the available space and plan for optimal utilization
- Consider future expansion needs
- Faculty Development
-
- Invest in training programs for faculty members
- Focus on healthcare simulation pedagogy, including:
-
-
- Clinical scenario development
- Effective debriefing techniques
-
-
- Ensure faculty understand the full potential of simulation technology
- Staffing Considerations
-
- Budget for essential personnel:
-
-
- Healthcare simulation technologists
- Program managers
- Administrative Staff
-
-
- Plan for ongoing training and professional development
- Equipment Selection and Maintenance
-
- Choose simulation equipment based on learning objectives and budget
- Consider a mix of high-fidelity and mid-fidelity patient simulators
- Plan for maintenance, repairs, and eventual replacement
- Factor in annual maintenance contracts and their costs
- Technology Integration
-
- Ensure robust IT infrastructure to support simulation technology
- Plan for integration with existing hospital or educational institution systems
- Operational Planning
-
- Develop protocols for equipment use and maintenance
- Create schedules for lab usage and maintenance
- Establish policies for safety and infection control
- Continuous Improvement
-
- Implement feedback mechanisms from learners and faculty
- Regularly review and update simulation scenarios and equipment
- Sustainability
-
- Develop a long-term plan for funding and resource allocation
- Consider the potential for revenue generation through external training programs
By carefully considering these factors, institutions can create effective and sustainable simulation labs that enhance medical education and ultimately improve patient care. Remember, the success of a simulation program depends not just on the equipment, but on how well it’s integrated into the curriculum and utilized by well-trained faculty.
Medical education – Robotic Surgery: What It Is, Examples, Benefits & Risks
A new intelligent collaborative post detailing this innovative medical technology will soon appear on my blogs.
Medical education – Outline of Normal Medical Education Program (6-7 Years)
The Foundation of Medical Education
Medical education typically has to follow a six to seven-year program, combining undergraduate and graduate studies. This integrated approach allows students to immerse themselves in medical training from the outset, providing a solid foundation for their future careers.
Pre-Medical Sciences
The first two years of the curriculum focus on basic sciences, laying the groundwork for more advanced medical studies. Students ought to delve into subjects such as:
- Biology
- Chemistry
- Physics
- Mathematics
- Anatomy
- Physiology
- Biochemistry
These courses will provide the essential knowledge needed to understand the complexities of the human body and disease processes.
Clinical Sciences
Years three and four introduce students to clinical sciences, bridging the gap between theoretical knowledge and practical application. Key subjects include:
- Pathology
- Pharmacology
- Microbiology
- Immunology
- Internal Medicine
- Surgery
- Pediatrics
- Obstetrics and Gynecology
During this phase, students begin to develop their clinical reasoning skills and learn to apply their knowledge to real-world medical scenarios.
Clinical Rotations
The final two to three years of the program will be dedicated to clinical rotations, where students gain hands-on experience in various medical specialties. These rotations typically include:
- Internal Medicine
- Surgery
- Pediatrics
- Obstetrics and Gynecology
- Psychiatry
- Family Medicine
- Emergency Medicine
Students will work alongside experienced physicians, learning to diagnose and treat patients under supervision.
Research and Community Health
Medical schools must emphasize research and community health as integral parts of their curriculum. Students often participate in research projects and community outreach programs, gaining valuable experience in public health and understanding the social determinants of health.
Specialization Options
Upon completing their general medical education, graduates can pursue specialization through residency programs. Popular specialties should include:
- Cardiology
- Neurology
- Oncology
- Pediatrics
- General Surgery
- Family Medicine
These specialization programs typically last 3-5 years, depending on the specialty chosen.
Medical education – Outline of Accelerated Medical Education Program (3-4 Years)
Here’s a detailed outline for an accelerated medicine curriculum (3-4 years) tailored for medical schools:
Accelerated Medical Education Program
Duration: 3-4 years
Year 1: Foundations of Medical Science
- Basic Sciences (6 months)
- Anatomy
- Physiology
- Biochemistry
- Genetics
- Histology
- Embryology
- Introduction to Clinical Medicine (3 months)
- Medical Ethics
- Patient Communication
- Physical Examination Skills
- Medical Spanish (or relevant local language)
- Pathophysiology and Pharmacology (3 months)
- General Pathology
- Introduction to Pharmacology
- Immunology
Year 2: Integrated Systems and Clinical Sciences
- Integrated Organ Systems (8 months)
- Cardiovascular
- Respiratory
- Gastrointestinal
- Renal and Urinary
- Endocrine and Reproductive
- Musculoskeletal
- Nervous System
- Clinical Sciences (4 months)
- Microbiology and Infectious Diseases
- Epidemiology and Biostatistics
- Nutrition and Metabolism
- Behavioral Sciences and Psychiatry
Year 3: Clinical Rotations and Community Health
- Core Clinical Rotations (8 months)
- Internal Medicine
- Surgery
- Pediatrics
- Obstetrics and Gynecology
- Family Medicine
- Community Health and Primary Care (2 months)
- Public Health
- Preventive Medicine
- Rural Health Outreach
- Research and Evidence-Based Medicine (2 months)
- Research Methodology
- Critical Appraisal of Medical Literature
Year 4 (Optional, for 4-year programs):
- Advanced Clinical Rotations (6 months)
- Emergency Medicine
- Critical Care
- Subspecialty Electives
- Preparation for Medical Practice (3 months)
- Advanced Clinical Skills
- Medical Licensing Exam Preparation
- Residency Application Support
- Capstone Project (3 months)
- Quality Improvement Project
- Community Health Initiative
Key Features:
- Integrated curriculum: Combining basic sciences with clinical applications from the start.
- Early clinical exposure: Introducing patient contact and clinical skills in the first year.
- Focus on primary care and community health: Addressing the specific needs of healthcare systems.
- Emphasis on cultural competence: Including training in medical Spanish or relevant local languages.
- Research component: Encouraging evidence-based practice and critical thinking.
- Flexibility: Offering both 3-year and 4-year options to accommodate different learning paces and career goals.
- Technology integration: Utilizing e-learning platforms and simulation labs to enhance learning efficiency.
- International collaboration: Partnering with institutions worldwide for exchange programs and global health perspectives.
This curriculum aims to produce competent physicians in an accelerated timeframe while addressing the specific healthcare needs and challenges of medical programs. It combines rigorous academic training with practical clinical experience and community engagement.
However, each country has its own legislation regarding the workload and duration requirements for medical courses. Many countries do not permit accelerated medical programs. Typically, they require a workload of 7,200 hours of theoretical and practical activities to obtain a Higher Education diploma and the title of medical Doctor.
The detailing of the workload of each subject will be completed in the following stages during the implementation of the teaching unit, following the legal guidelines required for each course.
In conclusion, normal and accelerated medical education programs should offer a comprehensive and integrated approach to training future physicians. With its focus on both theoretical knowledge and practical skills, combined with an emphasis on community health and research, medical schools must prepare students to become well-rounded and competent healthcare professionals ready to meet the challenges of modern medicine.