Contents
- 1 Exploring the Cutting-Edge Technology Transforming Operating Rooms
- 2 Prof. Aécio D’Silva, Ph.D AquaUniversity
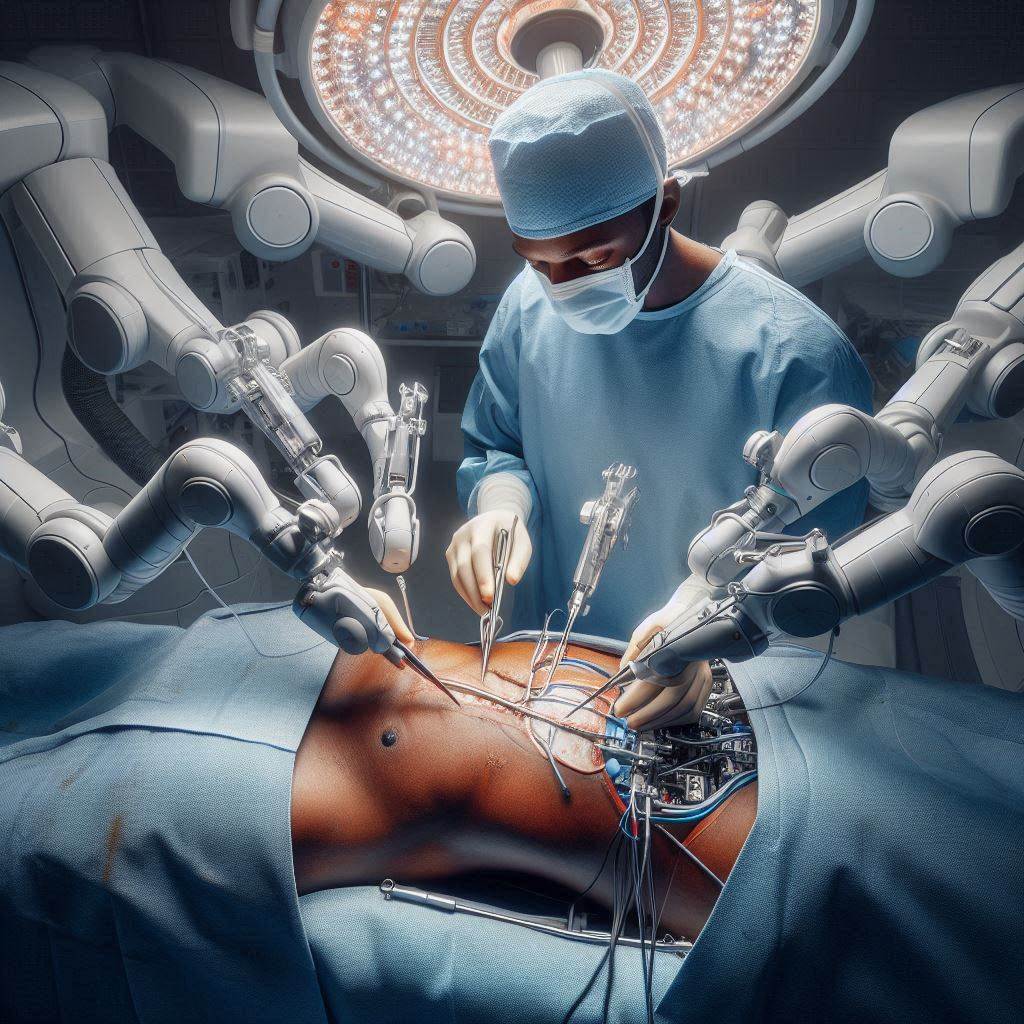
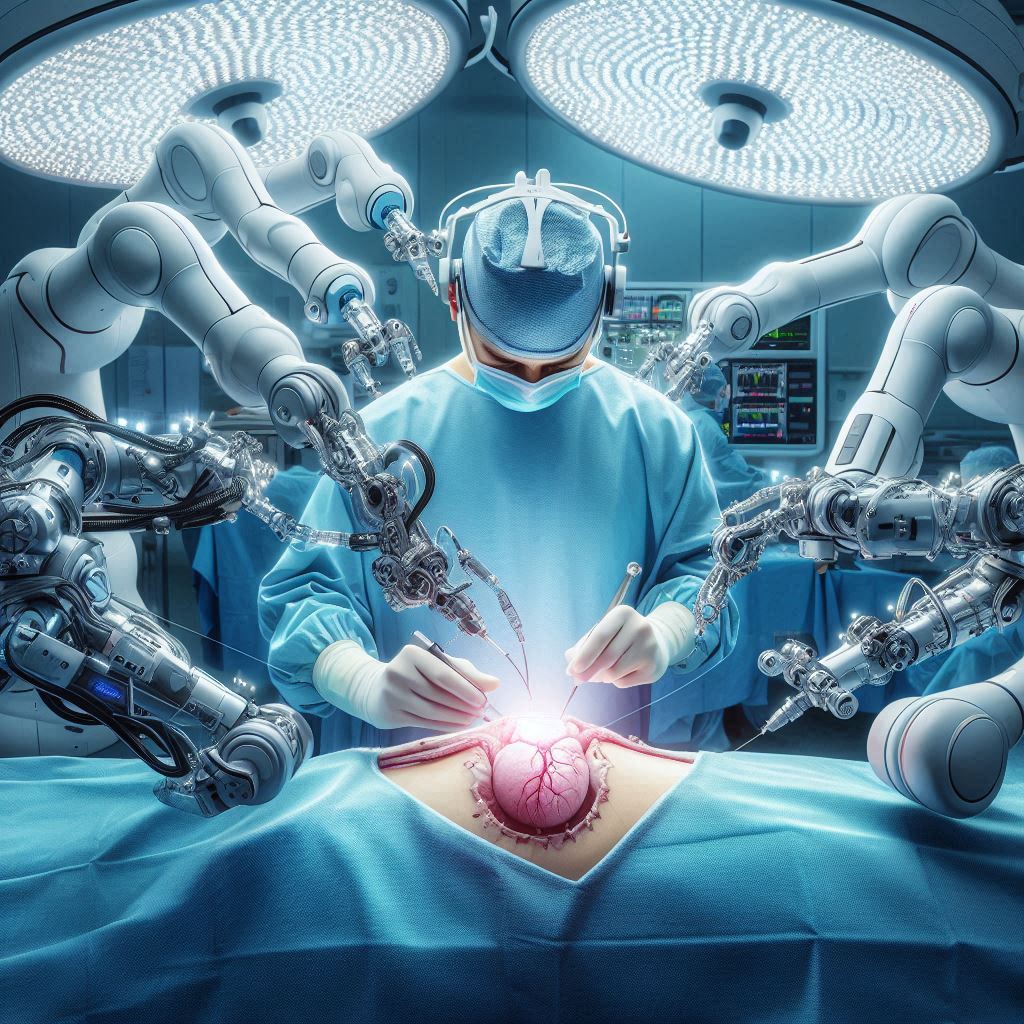
- 3 A surgeon operating a robotic surgical system, with multiple robotic arms performing precise movements on a patient
- 4 Understanding Robotic Surgery
- 5 Understanding Robotic Surgery
- 6 Common Examples of Robotic Surgery
- 7
- 8 Benefits of Robotic Surgery
- 9 Risks and Limitations
- 10 Future Developments in Robotic Surgery
- 11
- 12 How AI Algorithms Enhance the Autonomy of Surgical Robots:
- 13 How AI contributes to the automation of surgical tasks:
- 14 Best ways to train medical students to perform robotic-guided surgeries and procedures:
- 15 Ways AI Algorithms Can Be Integrated into Surgical Simulation Training
- 16 Use of VR-based Surgical E-Learning Techniques to Train Medical Students in Robotic Surgeries
- 17 How VR use in medical education helps build the confidence of medical students in performing surgeries
- 18 How VR enhances decision-making skills in medical students:
Exploring the Cutting-Edge Technology Transforming Operating Rooms
Prof. Aécio D’Silva, Ph.D
AquaUniversity
A surgeon operating a robotic surgical system, with multiple robotic arms performing precise movements on a patient
Robotic surgery has emerged as a revolutionary approach in modern medicine, offering surgeons enhanced precision and control during complex procedures. This advanced technology is transforming the landscape of minimally invasive surgery, providing patients with potential benefits such as shorter recovery times and reduced complications. This blog post will explore what robotic surgery entails, its applications, advantages, and potential risks.
Understanding Robotic Surgery
Robotic surgery, also known as robot-assisted surgery, involves the use of a computer-controlled robotic system to assist surgeons in performing complex procedures with greater precision and flexibility than traditional techniques allow.
Understanding Robotic Surgery
In robotic surgery, the surgeon sits at a console near the operating table, controlling robotic arms equipped with surgical instruments. The system translates the surgeon’s hand movements into precise, scaled-down movements of the instruments inside the patient’s body. High-definition 3D cameras provide a magnified, detailed view of the surgical site.
Common Examples of Robotic Surgery
Robotic surgery is used across various medical specialties, including:
– Urology: Prostatectomies and kidney surgeries
– Gynecology: Hysterectomies and fibroid removal
– Cardiothoracic: Heart valve repair and lung resections
– General surgery: Colorectal procedures and hernia repairs
Benefits of Robotic Surgery
Robotic surgery offers several potential advantages:
- Enhanced precision and dexterity
- Smaller incisions leading to less scarring
- Reduced blood loss and pain
- Shorter hospital stays and faster recovery times
- Improved visualization for surgeons
Risks and Limitations
While robotic surgery has many benefits, it’s important to consider potential risks:
- Higher initial costs for hospitals
- Longer operating times in some cases
- Limited tactile feedback for surgeons
- Potential for mechanical failures or malfunctions
- Learning curve for surgeons adapting to the technology
Future Developments in Robotic Surgery
The field of robotic surgery continues to evolve rapidly. Future advancements may include:
– Integration of artificial intelligence for surgical planning and guidance
– Improved haptic feedback systems
– Remote surgery capabilities for telemedicine applications
– Miniaturization of robotic systems for even less invasive procedures
Here are some real-world examples of robotic surgery in action:
- ROSA for Knee Surgery: ROSA (Robotic Surgical Assistant) is used for total knee arthroplasty (TKA) procedures. It helps surgeons perform precise bone preparation and implant positioning during knee replacement surgeries.
- Da Vinci Surgical System: Developed by Intuitive Surgical, this is one of the most widely used robotic surgery platforms. It’s used for various minimally invasive procedures across specialties like urology, gynecology, and general surgery. The system translates the surgeon’s hand movements into precise movements of miniaturized instruments inside the patient’s body.
- Senhance Surgical System: Created by Asensus Surgical, this system provides surgeons with enhanced control during laparoscopic procedures. It features an eye-controlled camera and haptic feedback to alert surgeons when they apply too much pressure during surgery.
- Smart Tissue Autonomous Robot (STAR): This system demonstrates a high level of autonomy in surgical procedures. It has been used in laparoscopic operations to create and execute surgical plans with minimal human intervention. STAR uses machine learning algorithms, 3D imaging, and computer vision to adapt to changes during surgery.
- Vicarious Surgical’s Robotic System: This system uses tiny human-like robotic arms equipped with 28 sensors per arm to mimic a surgeon’s movements. It allows for precise operations through very small incisions.
- ReWalk Robotics’ Personal Exoskeleton: While not a surgical robot per se, this is an example of robotic technology used in medical rehabilitation. It assists patients with spinal cord injuries in relearning how to walk.
- Robot-assisted heart surgery: As mentioned in the Mayo Clinic article, robotic systems are used in complex cardiac procedures, allowing surgeons to perform delicate operations with enhanced precision and control.
These examples showcase how robotic surgery is being applied across various medical specialties, from orthopedics and general surgery to cardiac procedures and rehabilitation, demonstrating the versatility and growing adoption of this technology in healthcare.
How AI Algorithms Enhance the Autonomy of Surgical Robots:
- Pattern recognition and adaptation:
– AI enables robots to learn surgical procedure patterns and replicate them with advanced precision.
– Robots can detect changes or abnormalities during surgery and adjust their actions in real-time.
– For example, a robot trained in tissue removal patterns can adapt if it detects tissue deformations during the procedure.
- Deep Learning for comprehensive planning:
– Deep Learning algorithms allow robots to incorporate data from pre- and post-operative stages.
– This enables robots to predict potential risks and complications based on patient-specific data.
– For instance, a robot can analyze pre-operative CT scans to predict risks of organ failure during the procedure.
- Computer vision for enhanced perception:
– AI-powered computer vision allows robots to recognize and classify surgical gestures and anatomical structures.
– This enables more accurate replication of complex surgical tasks.
– For example, robots can be trained to recognize and classify suturing gestures for precise execution.
- Autonomous decision-making:
– Advanced AI algorithms enable robots to make quick alterations to surgical plans in real-time.
– When unexpected issues arise during surgery, AI-enhanced robots can provide alternative solutions without manual reconfiguration.
- Adaptive learning:
– Systems like the Smart Tissue Autonomous Robot (STAR) use machine learning algorithms to adapt to changing conditions during surgery.
– These robots can generate and execute surgical plans with minimal human intervention, adjusting for tissue movement or deformation.
- Enhanced situational awareness:
– AI algorithms improve robots’ ability to track changes in the operating room, detect errors, and react to emergencies.
– This includes the ability to monitor patient vital signs and adjust surgical techniques accordingly.
- Predictive capabilities:
– AI-enhanced robots can predict tool trajectories and potential complications, allowing for proactive adjustments during surgery.
- Automated performance metrics:
– AI can analyze robot system data (kinematics, video, events) alongside postoperative outcomes to develop automated performance metrics.
– This enables objective evaluation of surgical skills and procedures.
These AI-driven enhancements significantly increase the autonomy of surgical robots, allowing them to perform more complex tasks with less direct human control while maintaining or improving precision and safety. However, it’s important to note that these systems still operate under human supervision, with surgeons maintaining ultimate control and decision-making authority.
How AI contributes to the automation of surgical tasks:
- Stepwise automation: AI algorithms are being developed to automate certain surgical tasks and steps, reducing the physical and mental workload on surgeons during procedures. This includes:
– Autonomous camera positioning on robotic surgical systems like the da Vinci robot.
– Automating repetitive subtasks by breaking down complex procedures into smaller steps that can be performed autonomously.
- Learning from demonstration (LfD):
– AI systems can learn surgical tasks by observing and imitating operations conducted by expert surgeons.
– This allows robots to be “trained” to conduct new tasks independently based on accumulated information from human demonstrations.
- Task segmentation and modeling:
– AI breaks down complex surgical procedures into several subtasks and basic gestures.
– It then recognizes, models, and conducts these subtasks sequentially, allowing for partial automation of procedures.
- Enhanced precision and control:
– AI-driven surgical robots can decrease fluctuations during surgery, improving precision beyond human capabilities for certain tasks.
– This allows surgeons to focus on more complex aspects of the surgery while routine tasks are automated.
- Real-time decision support:
– AI systems can provide real-time insights and guidance during procedures, such as identifying critical anatomical structures or suggesting optimal instrument trajectories.
- Autonomous performance of specific tasks:
– In some cases, AI systems have been developed to perform certain surgical tasks autonomously, such as suturing or tissue removal, under human supervision.
- Adaptive learning:
– AI systems can continuously learn and improve their performance based on data from multiple procedures, potentially surpassing human consistency in specific tasks.
While these advancements show significant progress in automating aspects of surgery, it’s important to note that full automation of complex surgical procedures is still far from reality. The goal is to augment and assist human surgeons rather than replace them entirely. Ethical considerations and the need for human oversight remain crucial as these technologies develop.
Best ways to train medical students to perform robotic-guided surgeries and procedures:
- Simulation-based training:
– Use virtual reality simulators and robotic surgery simulators to provide hands-on experience without risk to patients.
– This allows students to practice basic skills and become familiar with robotic controls in a safe environment.
- Graduated responsibility:
– Start with observing robotic procedures, then assisting, and gradually progressing to performing parts of procedures under supervision.
– This stepwise approach allows students to build confidence and skills over time.
- Structured curriculum:
– Develop a comprehensive curriculum that covers both theoretical knowledge and practical skills.
– Include modules on robotic system components, setup, troubleshooting, and specific surgical techniques.
- Integration with traditional surgical training:
– Ensure students have a strong foundation in anatomy, surgical principles, and traditional open surgical techniques before advancing to robotic surgery.
- Mentorship and proctoring:
– Pair students with experienced robotic surgeons for one-on-one guidance and feedback.
– Implement a structured proctoring program for supervised practice.
- Video review and analysis:
– Use recorded robotic surgeries for detailed analysis and discussion of techniques, decision-making, and potential improvements.
- AI-enhanced feedback:
– Utilize AI algorithms to provide objective assessments of surgical skills and performance metrics.
– This can help identify areas for improvement and track progress over time.
- Interdisciplinary training:
– Include training on teamwork and communication with other OR staff, as robotic surgery requires effective collaboration.
- Hands-on lab experience:
– Provide access to robotic systems in a laboratory setting for practice outside of actual surgeries.
- Continuing education:
– Emphasize the importance of ongoing learning and skill development, as robotic technology continues to evolve.
- Ethics and decision-making training:
– Include modules on the ethical considerations of robotic surgery and when to convert to open procedures if necessary.
- Assessment and certification:
– Implement rigorous assessment methods to ensure competency before allowing independent practice.
– Consider formal certification programs for robotic surgery skills.
By combining these approaches, medical schools can provide comprehensive training that prepares students for the complexities of robotic-guided surgeries while ensuring patient safety remains the top priority.
Ways AI Algorithms Can Be Integrated into Surgical Simulation Training
- Performance evaluation and feedback:
– AI algorithms can analyze trainee performance during simulated procedures and provide personalized feedback.
– For example, machine learning algorithms have been developed to classify participants’ skill levels during VR-based surgical tasks and provide feedback compared to expert benchmarks.
- Enhanced simulation environments:
– AI can generate complex, dynamic virtual environments and patient-specific anatomical models for more realistic training scenarios.
– This allows trainees to practice on a wider variety of simulated cases.
- Predictive modeling:
– AI can analyze historical performance data to predict trainees’ future performance and skill development trajectories.
– This enables personalized training plans and early identification of trainees needing additional support.
- Augmented reality guidance:
– AI-powered augmented reality tools can provide real-time visual cues and information during simulated procedures to enhance learning.
- Automated assessment:
– Machine learning algorithms can be used to automatically assess surgical skills and techniques based on motion data and video analysis.
- Virtual surgical assistants:
– AI-powered virtual assistants can provide guidance and answer questions during simulations.
- Personalized learning:
– AI can tailor simulation scenarios and difficulty levels to individual trainee needs and skill levels.
- Video analysis:
– AI systems can analyze recordings of simulated procedures to provide detailed feedback on techniques and identify areas for improvement.
- Natural language processing:
– NLP algorithms can be used to transcribe, translate, and summarize verbal feedback from instructors during simulations.
- Objective skill assessment:
– AI enables more standardized and objective assessment of surgical skills compared to traditional subjective evaluations.
To effectively integrate these AI capabilities, surgical simulation platforms need to incorporate machine learning models, computer vision, natural language processing, and other AI technologies. Standardization of AI implementation and large datasets for training algorithms remain key challenges. Overall, AI has significant potential to enhance the realism, personalization and effectiveness of surgical simulation training.
Use of VR-based Surgical E-Learning Techniques to Train Medical Students in Robotic Surgeries
The use of VR-based surgical techniques to train medical students in robotic surgeries appears to be quite efficient and beneficial. Here are some key points highlighting the efficiency of this approach:
- Immersive and realistic training:
– VR provides a fully immersive, simulated experience that closely replicates real-world surgical scenarios].
– Students can practice complex procedures in a realistic 3D environment, enhancing their understanding of spatial relationships and surgical techniques [2][3].
- Standardized and accessible learning:
– VR-based training offers standardized educational experiences that can be accessed remotely, at any time .
– This accessibility allows for consistent training quality across different locations and institutions [1].
- Safe practice environment:
– VR allows students to make mistakes and learn from them without risking patient safety.
– This safe environment encourages deliberate practice and experimentation, which can accelerate skill development.
- Repeated practice and feedback:
– Students can perform procedures multiple times, unlike in traditional cadaver or bio skills labs where opportunities are limited.
– Many VR systems provide real-time evaluation and feedback on performance, allowing for immediate improvement.
- Enhanced visualization and understanding:
– VR can provide unique perspectives, such as first-person views of surgical procedures, which are difficult to achieve in traditional training.
– The technology allows for detailed exploration of human anatomy in 3D, improving students’ understanding.
- Skill assessment and personalized learning:
– AI algorithms integrated into VR simulations can assess surgical skills and provide personalized feedback.
– This enables tailored learning experiences and helps identify areas for improvement.
- Cost-effective and resource-efficient:
– Once developed, VR simulations can be used repeatedly without additional material costs, unlike traditional methods that require ongoing resources (e.g., cadavers, equipment).
- Preparation for robotic surgery:
– VR simulations can specifically target skills needed for robotic surgery, such as hand-eye coordination and 3D spatial awareness.
– AI-enhanced VR can provide visual cues and warnings based on predicted tool trajectories, improving situational awareness for robotic procedures.
- Accelerated learning curve:
– The combination of immersive practice, immediate feedback, and AI-enhanced guidance can potentially accelerate the learning curve for both traditional and robotic surgical techniques.
While VR-based surgical e-learning shows great promise, it’s important to note that it should complement, not replace, other forms of medical education. Technology is still evolving, and more research is needed to fully quantify its long-term impact on surgical proficiency. However, the current evidence suggests that VR-based training is an efficient and effective tool for preparing medical students for robotic and traditional surgical procedures.
How VR use in medical education helps build the confidence of medical students in performing surgeries
- Safe practice environment:
– VR allows students to practice surgical procedures repeatedly without risk to real patients.
– This safe environment encourages experimentation and learning from mistakes, which builds confidence over time.
- Realistic simulations:
– VR provides immersive, 3D environments that closely replicate real surgical scenarios.
– This helps students become familiar with the surgical environment and procedures before encountering them in real life.
- Repeated practice:
– Unlike traditional methods (e.g., cadaver labs), VR allows for unlimited repetitions of procedures.
– This repetition helps build muscle memory and procedural confidence.
- Immediate feedback:
– Many VR systems provide real-time feedback on performance, allowing students to identify and correct mistakes immediately.
– This rapid feedback loop accelerates learning and builds confidence in skills.
- Objective assessment:
– VR systems can provide objective metrics on performance, allowing students to track their progress over time.
– Seeing measurable improvement can significantly boost confidence.
- First-person perspective:
– VR can provide unique viewpoints, such as a surgeon’s eye view, which are difficult to achieve in traditional training.
– This perspective helps students better understand spatial relationships and surgical techniques.
- Stress management:
– By simulating high-pressure scenarios in a controlled environment, students can learn to manage stress associated with surgery.
– This stress inoculation can increase confidence when facing real surgical situations.
- Procedural familiarity:
– VR allows students to become familiar with the steps of various surgical procedures before performing them on real patients.
– This familiarity reduces anxiety and increases confidence when transitioning to real surgeries.
- Diverse case exposure:
– VR can simulate a wide range of surgical cases, including rare conditions, giving students confidence in handling various scenarios.
- Self-paced learning:
– Students can progress at their own pace in VR, building confidence gradually as they master each skill level.
- Visualization of complex anatomy:
– VR can provide detailed, 3D visualizations of anatomy, improving students’ understanding and confidence in navigating complex structures during surgery.
- Team training:
– Some VR systems allow for multiplayer scenarios, helping students build confidence in their role within a surgical team.
By providing these benefits, VR helps medical students build confidence in their surgical skills in a safe, controlled environment before they enter the operating room with real patients. This increased confidence can lead to better performance and potentially improved patient outcomes when students transition to real-world surgical practice.
How VR enhances decision-making skills in medical students:
- Realistic scenario simulations:
– VR provides immersive, true-to-life environments that replicate real clinical scenarios.
– This allows students to practice making decisions in contexts very similar to what they’ll face in real medical situations.
- Safe practice environment:
– VR allows students to make critical decisions without risking patient safety.
– This encourages students to take risks and learn from mistakes, which is crucial for developing decision-making skills.
- Immediate feedback:
– Many VR systems provide real-time feedback on decisions made during simulations.
– This immediate feedback helps students understand the consequences of their choices and refine their decision-making process.
- Repeated practice:
– VR enables students to practice decision-making in various scenarios repeatedly.
– This repetition helps build confidence and improves decision-making speed and accuracy over time.
- High-pressure situation training:
– VR can simulate emergency and trauma scenarios, allowing students to practice quick decision-making under pressure.
– This helps prepare students for high-stress situations they may encounter in real medical practice.
- Diverse case exposure:
– VR can simulate a wide range of medical cases, including rare conditions.
– This broad exposure helps students develop more comprehensive decision-making skills across various medical situations.
- Objective assessment:
– VR systems can track and analyze students’ decision-making processes objectively.
– This data can be used to identify areas for improvement and tailor training to individual needs.
- Time-critical decision training:
– As mentioned in the Johns Hopkins example, VR can incorporate AI that adapts to students’ actions, forcing them to make time-critical decisions.
– This helps students learn to make quick, effective decisions under time pressure.
- Visualization of consequences:
– VR can visually demonstrate the outcomes of decisions, helping students better understand the impact of their choices.
- Team-based decision-making:
– Some VR systems allow for multiplayer scenarios, helping students practice collaborative decision-making in a medical team context.
- Standardized training:
– VR provides a standardized environment for decision-making practice, ensuring all students have access to the same high-quality training scenarios.
By providing these benefits, VR helps medical students develop and refine their decision-making skills in a safe, controlled environment before they face real-life clinical situations. This enhanced decision-making ability can lead to better patient outcomes when students transition to real-world medical practice.
In conclusion, robotic surgery represents a significant leap forward in surgical technology, offering numerous benefits for both patients and surgeons. While challenges remain, ongoing research and development promise to further refine and expand the capabilities of robotic surgical systems. As this technology continues to advance, it has the potential to revolutionize surgical care, improving outcomes and accessibility for patients worldwide.
References:
- Intuitive Surgical. (2023). da Vinci Surgery. https://www.davincisurgery.com/
- Ghezzi, T. L., & Corleta, O. C. (2016). 30 Years of Robotic Surgery. World Journal of Surgery, 40(10), 2550-2557.
- Lanfranco, A. R., Castellanos, A. E., Desai, J. P., & Meyers, W. C. (2004). Robotic Surgery: A Current Perspective. Annals of Surgery, 239(1), 14-21.
- Peters, B. S., Armijo, P. R., Krause, C., Choudhury, S. A., & Oleynikov, D. (2018). Review of emerging surgical robotic technology. Surgical Endoscopy, 32(4), 1636-1655.
- https://www.anl.gov/cels/using-ai-to-enhance-robotic-surgery-and-improve-patient-outcomes
- https://news.ecu.edu/2024/01/22/robot-surgery-research/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10907451/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10508667/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10389387/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9975916/
- https://elarasystems.com/medical-training-advances-to-vr/
- https://medvr.education